Warts
What are Warts?
Warts are among the most common, persistent, and frustrating conditions that we see on a daily basis in our dermatology office. Described throughout recorded human history, they affect both children and adults alike. Without treatment (sometimes even with treatment) they can persist for months, even years.

What Causes Warts?
Warts, or verrucae, are a viral infection of the skin, caused by the human papillomavirus (HPV). There are over 100 known HPV types, and the virus can infect almost any area of the skin. Probably the most common areas are the feet (known as ‘plantar warts”) and hands, but in our office, we certainly see them on many other areas such as elbows and knees, the face, or the genital area (where they are known as ‘condyloma’).
Infection occurs when the skin comes into contact with the virus, whether from a surface (like a health club shower floor) or from another person; the virus infects the skin cells, which then form a visible skin lesion. From an original site on the skin, the virus can spread locally to adjacent areas, or be transferred to distant sites, such as when someone scratches or picks at a wart and then touches another part of the skin. Since the virus must live inside the cells on the surface of the skin, they cannot travel internally to the rest of the body.

Who Gets Warts?
They are extremely common in children, but can also be seen in adults of any age. Certain individuals seem to pick them up much more easily (and develop a greater number of warts) than others, leading to the thought that some people have less of a natural immunity to the human papillomavirus specifically (not to all infections). Modern medicine has also led to a category of people who regularly take medications that suppress the immune system, and these patients are also more likely to develop warts, possibly many of them.
Wart Treatment
Treatment of warts comes in many forms, and here is where the frustration begins! There are no medications that directly kill HPV, and the virus is very good at resisting our efforts to eradicate it. Frequently a person’s natural immune system at some point kicks in and takes care of them on its own, but there is no way to predict in any one person how long this will take. There is a vaccination currently available (Gardasil®) for young women and men to protect them against the sexually transmitted form of human papillomavirus that causes some forms of genital warts (condyloma) and cervical cancer. There is currently no vaccination against common warts. In centuries past there have been some rather bizarre approaches to treating warts, such as applying spider webs or pork fat to the affected skin or using magic words.

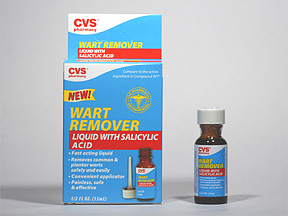
Currently, there are a few over the counter remedies: salicylic acid application, freezing equipment, and duct tape. Salicylic acid works by exfoliating the infected skin cells but can take a lot of time to see improvement. Over-the-counter freezing products, which contain dimethyl ether and propane (a common refrigerant) cool the affected skin to negative 57 degrees and cause the wart area to slough away. While this treatment can be helpful, it may be painful to use and difficult to self administer. The mechanism of duct tape is unknown, though it may help by irritating or warming the area, and its benefit is limited (about 1 in 5 people improve).
In our office, we have a number of approaches to treating warts. The ideal treatment would be very effective, with minimal discomfort and minimal risk of scarring. While this ideal may be difficult to obtain, we use our best efforts to tailor our treatment to what is best for each patient. Most commonly, we use liquid nitrogen; with a temperature of negative 200 degrees, it essentially damages the wart infected skin. Unfortunately, it causes some discomfort and often requires multiple treatments. An alternative choice is called Cantharidin, a topical medication derived from the so-called “blister beetle”. Sometime after application, it causes blistering in the skin, hopefully killing the wart infected skin away as it heals. It also usually requires multiple treatments. We occasionally use one of our vascular lasers to target the blood supply in the wart, which some patients find effective. There is some discomfort involved in laser treatment, multiple treatments are needed, and the laser itself is very expensive. Finally, we can treat resistant warts with an injection of Candida proteins. A series of 3 (unfortunately painful) treatments can stimulate an immune reaction at the site of the wart to kill it. There are also a number of prescription creams that have been used to treat warts including Fluorouracil and Imiquimod. They generally cause less discomfort than many in-office treatments, but their use often requires weeks or months and may not work for everyone.
Many of our patients ask us (often in frustration) if warts can be surgically removed. The answer is yes, and there are times when this is a reasonable option. The procedure can be performed under a local anesthetic and may result in the eradication of the wart. However, with this treatment comes discomfort, the risk of lifelong scarring, as well as the possibility that the wart may still recur.
What To Do If You See A Wart On Your Skin
1. If the wart is rapidly growing, painful, or bleeding make sure you seek a physician’s opinion as it may be something else entirely.
2. Try over-the-counter salicylic acid wart remover. Particularly helpful is the liquid, though patches and bandaids containing salicylic acid are available.
3. Use duct tape. This works very well applied on top of the liquid wart remover every night. If you are pregnant, or if the wart is on a young child, try the duct tape alone and replace it daily.
4. Don’t pick or touch your warts, as this can spread them.
5. If the warts are winning the battle after 6 weeks of diligent home treatment, see your local dermatologist for other options.
Warts have been with humans for thousands of years, and their treatment is a daily challenge for those of us in dermatology, as well as our patients who suffer with them. Someday, we hope to have a “magic bullet” for these stubborn lesions. Until then, we will continue to work with our patients to determine which treatment or combination of treatments will work best for them.

